A 47 YEAR OLD MALE WITH PAIN IN THE ABDOMEN SINCE 3 YEARS .
This is an an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input
Rahul Tangellamudi
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitted.
CONSENT WAS GIVEN BY BOTH PATIENT AND ATTENDERS
CASE PRESENTATION:-
Patient came to the casualty with complaints of pain in the abdomen (epigastric region) since 3 years
HISTORY OF PRESENTING ILLNESS:-
Patient was apparently asymptomatic 3 yrs back .he used to get episodes of pain which is insidious in onset , intermittent in nature,dragging type, non radiating, aggravated on consumption of alcohol relieved on taking medication .
15 days ago Pt brought to OP due to back pain (no stomach pain) increased intensity relieved on medication and advised exercises .
10 days ago pt went to a close members reception and had indulged himself in alcohol nearly 1.5 litres of whiskey and mutton . Then next day when he woke up he started experiencing pain in the abdomen in the epigastric region . Intermittent in nature ,insidious in onset , non radiating . He was unable to move . He was brought to hospital by the help of his family members .
He also had 2 to 3 episodes of vomitings ( white with yellowish discolouration ( bile) ) .
Pt is also experiencing shortness of breath since 4 to 5 years ( grade 1 ) .
No h/o fever
No h/o headache, redness of eyes.
No h/o dysphagia, throat pain.
No h/o burning micturition.
No h/o bleeding manifestations.
PAST HISTORY:-
N/k/c/o. HTN ,epilepsy, thyroid disorders, CAD, CVA.
Pt has no idea he has diabetes until he got admitted in hospital due to abdominal pain and got checked
Pt is diagnosed with type 3c diabetes.
PERSONAL HISTORY:-
Diet - mixed
Appetite- decreased
Bowel and bladder- regular
Sleep- not adequate
Addictions- pt is chronic alcoholic . He started drinking at the age of 24 . Initially he started it as fun . Later he got addicted . Pt is been drinking daily half litre of whiskey since 25 years . He also chronic tobacco abuser . He eats a total of 15 gutka packets daily .
Pt is a lorry driver . So his diet and sleep is all disturbed and he is the sole bread earner in his family with three kids and a wife.
Current occupation - ELECTRICIAN
DAILY ROUTINE:-
6.30 : wakes up.
7-8 am: breakfast sometimes he will skip
8-1 pm : drives lorry
1-1 30 : lunch mostly outside
1 30- 2 30: takes rest
2 30 - 9 30 drives lorry
9 30 - 10 : dinner mostly outside
10 - 6 30 am : rest
GENERAL EXAMINATION:-
Patient is conscious, coherent, cooperative, moderately built and nourished.
Pallor present.
No icterus, cyanosis, clubbing, lympadenopathy, edema.
VITALS:-
Temperature - afebrile
BP- 130/90 mmhg
PR- 82bpm
RR- 22 cpm
GRBS- 113mg/dl.
Spo2- 96%
SYSTEMIC EXAMINATION:-
P/A-
Inspection :
Shape of the abdomen - obese
Umbilicus - inverted
Skin - no scars , no sinuses , no dilated veins
All quadrants moving uniformly , no visible peristalsis
Palpitation :
No local rise of temperature
Tenderness present in the epigastrium
Abdomen is soft
No hepatomegaly no spleenomegaly
Percussion :
Tympanic note heard in all quadrants
Auscultation :
Bowel sounds heard
CVS - s1 s2 heard , no murmurs or thrills
RS- b/l , NVBS heard , no added sounds
CNS- NFND
FEVER CHARTING:-
ECG:
USG:-
Urine culture :-
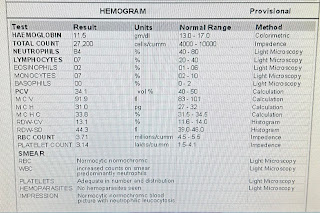
Hemogram:-
14-4-24
15-4-24
15-4-24 6pm
16-4-24
17-4-24
18-4-24
19-4-24
20-4-24
21-4-24
22-4-24
23-4-24
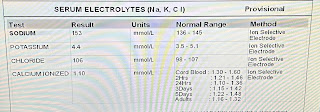
SERUM ELECTROLYTES:-
14-4-24
15-4-24
16-4-24
18-4-24
20-4-24
21-4-24
22-4-24
23-4-24
24-4-24
LIVER FUNCTION TESTS :-
14-4-24
18-4-24
19-4-24

















































Comments
Post a Comment