17 year old female with fever since 1 month, knee pain since 1 month, cough with sputum since 1 week.
This is an an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input
Rahul Tangellamudi
ROLL NO:-199
UNIT-I
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
The patient/ attender was informed the purpose of the information being acquired. An informed consent was taken from patient/ attender and there is omission of information that was requested to be omitted.
CONSENT WAS GIVEN BY BOTH PATIENT AND ATTENDERS
CASE PRESENTATION:-
Patient came to the casualty with complaints of fever since 1 month, knee pain since 1 month, cough with sputum since 1 week.
HISTORY OF PRESENTING ILLNESS:-
Patient was apparently asymptomatic 1 month back, then she developed low grade fever- evening rise of temperature, intermittent type , associated with chills .
She complains of knee joint pains , which is dull aching , non progressive, , no aggravating and relieving factors.
Cough With sputum of minimal quantity, white in colour, thin texture.
She came home for holidays 1 month back.Then after next day of Dusshera she developed fever and weakness for which she went to a local RMP and the RMP told that she has typhoid (no documents) and was given medications( no documents).
She was feeling alright for the next 1 week , then again she developed fever for which she again visited the same RMP and this time the RMP told that she has some blood infection (no documents) and was given medication(no documents).
This time the fever didn't subside .Then she visited a private hospital and investigations were done, but her complaints were not subsided for which she came to our hospital.
No h/o headache, redness of eyes.
No h/o dysphagia, dyspnoea, throat pain.
No h/o abdominal pain, burning micturition.
No h/o bleeding manifestations.
PAST HISTORY:-
N/k/c/o. DM, HTN ,epilepsy, thyroid disorders, CAD, CVA.
PERSONAL HISTORY:-
Diet - mixed
Appetite- decreased
Bowel and bladder- regular
Sleep- adequate
Addictions- none.
DAILY ROUTINE:-
6.30 : wakes up.
7-8 am: breakfast
8-9 am: gets ready to college.
9-9.15am :- prayer
9.15- 1 pm: class
1-2 pm:lunch
2-5 pm: class
5-6pm:takes bath and washes clothes
6-7.30 pm: study hour
7.30-8 pm - games
8-9 pm- dinner.
9 pm : goes to bed.
MENSTRUAL HISTORY:-
Age of menarche- 13 years.
28/5 ,regular .
GENERAL EXAMINATION:-
Patient is conscious, coherent, cooperative, moderately built and nourished.
Pallor present.
No icterus, cyanosis, clubbing, lympadenopathy, edema.
VITALS:-
Temperature - 100 F
BP- 90/60 mmhg
PR- 92 bpm
RR- 22 cpm
GRBS- 86 mg/dl.
SYSTEMIC EXAMINATION:-
CVS- S1, S2 heard, no murmurs
RS- b/l AE +, NVBS heard.
P/A- soft , non tender ,no organomegaly.
CNS- NFND.
FEVER CHARTING:-
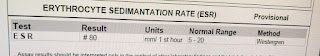
INVESTIGATIONS:-
ECG-
Chest x-ray-
2d-echo-






























Comments
Post a Comment